The Ultimate Guide to Managing and Treating Psoriasis in 2016
2016 Psoriasis Patients
Psoriasis is a chronic autoimmune disease that affects the skin, causing red, scaly patches. It affects an estimated 2-3% of the global population, with varying degrees of severity and impact on quality of life. Staying informed about the latest developments in psoriasis management is essential for both patients and healthcare professionals. This comprehensive guide aims to provide valuable insights and expert advice on managing psoriasis in 2016, highlighting the latest treatment options, lifestyle modifications, and support networks available to psoriasis patients.
Understanding Psoriasis in 2016
Psoriasis is a chronic inflammatory skin condition that is characterized by red, scaly patches known as plaques. It is a non-contagious condition that can occur anywhere on the body, although it is most commonly found on the elbows, knees, scalp, and lower back. Psoriasis is thought to be caused by a combination of genetic and environmental factors, with triggers including stress, infections, certain medications, and changes in weather.
*Prevalence of psoriasis*
Psoriasis affects approximately 2-3% of the global population, with varying degrees of severity. It can occur at any age, although it often develops between the ages of 15 and 35. Both men and women are affected equally, and psoriasis can occur in people of all races and ethnicities.
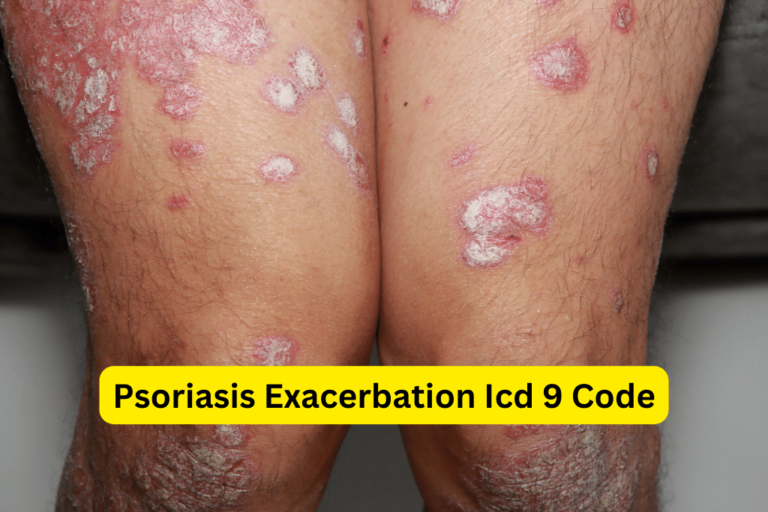
*Types of psoriasis and their characteristics*
There are several different types of psoriasis, including plaque psoriasis, guttate psoriasis, inverse psoriasis, pustular psoriasis, and erythrodermic psoriasis. Each type has its own unique characteristics and may require different treatment approaches. Plaque psoriasis is the most common form and is characterized by raised, red patches covered with a silvery-white build-up of dead skin cells.
*Triggers and risk factors associated with psoriasis development*
While the exact cause of psoriasis is unknown, several triggers and risk factors have been identified that may contribute to its development. These include a family history of psoriasis, viral or bacterial infections, stress, certain medications (such as beta blockers and lithium), and smoking.
*Common misconceptions about psoriasis*
There are many misconceptions surrounding psoriasis, leading to stigma and misunderstanding. It is important to dispel these misconceptions and educate others about the true nature of psoriasis. Some common misconceptions include the belief that psoriasis is contagious, that it is solely a skin condition, and that it is caused by poor hygiene.
Latest Treatment Options for Psoriasis in 2016
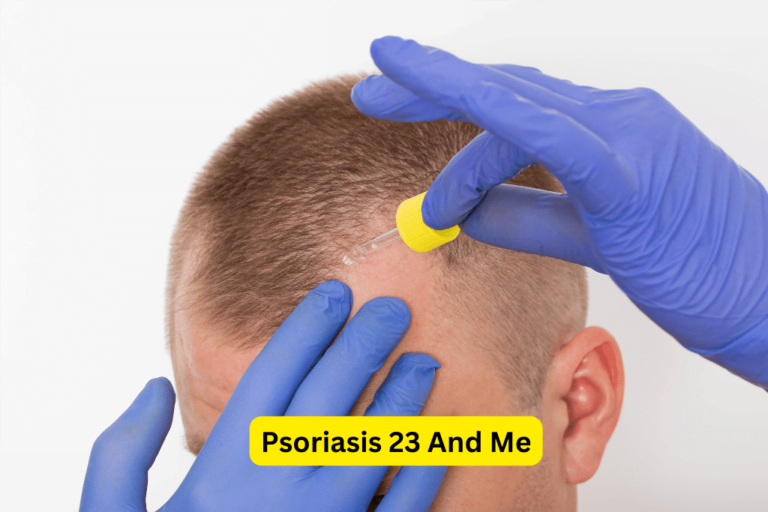
Topical Treatments
Topical treatments are often the first line of defense in managing psoriasis symptoms. These include corticosteroids, retinoids, coal tar-based creams, vitamin D analogues, and calcineurin inhibitors. Corticosteroids are frequently prescribed for their anti-inflammatory properties, while retinoids help to normalize skin cell growth. Coal tar-based creams can reduce inflammation, itching, and scaling. Vitamin D analogues can slow down cell growth and reduce inflammation, while calcineurin inhibitors are used primarily in sensitive areas of the skin.
Phototherapy and Light-Based Treatments
Phototherapy involves exposing the skin to ultraviolet (UV) light to reduce inflammation and slow down skin cell growth. There are different types of phototherapy available, including narrowband UVB, broadband UVB, and PUVA (psoralen plus UVA). Laser therapy is also a light-based treatment option that targets specific areas of the skin and can provide relief from psoriasis symptoms.
Systemic Medications
In more severe cases of psoriasis, systemic medications may be prescribed. These can include oral medications, such as methotrexate, cyclosporine, and apremilast, which work by suppressing the immune system. Biologic therapies are another type of systemic medication that target specific molecules involved in the immune system response. These include TNF inhibitors, IL-23 inhibitors, and IL-17 inhibitors. It is important to note that these medications may have potential side effects and require regular monitoring by a healthcare professional.
Alternative and Complementary Treatments
While there is no cure for psoriasis, many individuals find relief through alternative and complementary treatments. These can include natural remedies, such as aloe vera and fish oil, which have anti-inflammatory properties. Diet and nutrition can also play a role in managing psoriasis symptoms, with some evidence suggesting that a healthy diet rich in fruits and vegetables can help reduce inflammation. Alternative therapies, such as acupuncture and meditation, may also provide relief from stress and improve overall well-being.
Lifestyle Modifications for Managing Psoriasis in 2016
In addition to medical treatments, lifestyle modifications play a crucial role in managing psoriasis. Maintaining a healthy lifestyle, including regular exercise, proper skincare routines, and stress management, can help reduce psoriasis symptoms and improve overall well-being. It is also important to avoid smoking and excessive alcohol consumption, as these can exacerbate psoriasis symptoms. Dietary choices can also have an impact on psoriasis, with some individuals reporting improvements after eliminating certain trigger foods. Lastly, seeking support from friends, family, and support groups can provide emotional support and help individuals cope with the challenges of living with psoriasis.
Coping with Psoriasis: Insights from Real Patients
Living with psoriasis can be challenging, both physically and emotionally. Hearing real stories and experiences from individuals who have successfully managed their psoriasis can provide hope and inspiration. These personal accounts can shed light on the strategies and coping mechanisms employed by psoriasis patients. Building a network of understanding individuals and seeking emotional support from friends, family, and support groups can also make a significant difference in managing the psychological impact of psoriasis. Online communities and support groups specifically catered to psoriasis patients provide a platform for connection, information sharing, and emotional support.
Conclusion
Psoriasis is a complex condition that requires a multi-faceted approach to management and treatment. By staying informed about the latest developments in psoriasis management, individuals can make empowered decisions about their own health. It is essential to consult with healthcare professionals for personalized treatment plans based on individual needs and medical history. The future of psoriasis management holds promise, with ongoing research and advancements in treatment options. With the right support, education, and resources, individuals living with psoriasis can lead fulfilling lives and effectively manage their symptoms.
"Have You Seen Mike Walden's new holistic acne System yet? It's called "Acne No More" I've read the whole thing (all 223 pages) and there's some great information in there about how to naturally and permanently eliminate your acne without drugs, creams or any kind of gimmicks. I highly recommend it - it's very honest and straightforward without all the hype and b.s. you see all over the net these days. Here's the website where you can get more information:
Click Here -->AcneNoMore